Brachytherapy, or internal radiation therapy, refers to the placement of a radiation source close to or into the tumor through the insertion of applicators into the body. This is different from external beam radiation (EBRT) where radiotherapy is delivered from outside the body with a beam of radiation. Brachytherapy is used to treat cancer sites such as cervix, uterus, vagina, prostate, breast, and skin cancers. Depending on the clinical scenario, it can be used alone on in combination with other treatments such as EBRT, surgery, or chemotherapy.
Brachytherapy

There are several advantages of brachytherapy over EBRT; firstly, because the applicators are placed close to the tumor, radiation sources with a short range of effect can be used. In physics terms, this property is called a steep dose gradient, where there is a sharp fall-off of radiation dose within a few centimeters from the source. This means that any normal organs surrounding the targeted tumor will receive significantly reduced or no radiation dose. Secondly, the steep dose gradient with brachytherapy also allows high doses to be delivered to the tumor, providing an effective way for treatment to be delivered to smaller tumors.
Finally, if the patient moves during treatment, the brachytherapy applicators retain their position in relation to the tumor, ensuring consistent and accurate treatment delivery. This may not be the case with EBRT where there is a small chance the tumor may move out of the treatment beam.
Brachytherapy for Gynaecological Cancers
One of the commonest uses of brachytherapy is in the treatment of gynaecological cancers. The uterus and cervix are ideally suited for brachytherapy due to their easy accessibility through the vaginal canal, and their relatively consistent anatomy allowing the placement of standardized applicators for treatment. In addition, the close proximity of critical pelvic organs such as the bladder and rectum makes the steep dose fall off in brachytherapy a property that can be harnessed effectively to minimize damage to these normal tissues.
Multi-Channel or “Complex” brachytherapy
When used in the radical treatment of cervical or uterine cancer (ie without surgery), multi-channel brachytherapy is used to deliver a highly focused dose of radiation to the tumor usually after a course of external beam radiation. The term “multi-channel” refers to the use of several applicators inserted through the vagina in order to place the radiation sources close to the cervical or uterine tumor.
Figure 1 below shows the three brachytherapy applicators – 2 ovoids and 1 central tandem, commonly used in the curative treatment of cervical cancer. Each applicator has a hollow channel within it for a tiny radiation source to be threaded during treatment for varying amounts of time (dwell times). The shape and magnitude of the dose delivered to the tumor can then be customized by varying the dwell time of the radiation source at different points along the applicator (ie longer dwell time = higher dose).

Figure 1 – Applicators used in complex brachytherapy. The colored applicators are the ovoids which come in different sizes to fit varying sizes of the vaginal cavity, while the long tandems come in different lengths and angles to fit the shape of the uterus.
During the insertion of applicators, moderate sedation and painkillers will be administered to the patient to make the process as comfortable as possible. First, the tandem will be passed through the opening of the cervix and then up through the cavity of the uterus. Next, the 2 ovoids will be inserted to the right and left upper end of the vagina adjacent to the tandem. Once all applicators are in place, sterile gauze will be placed below and beside the applicators as a final step to fill the air gaps between the applicators so that dose calculations will be accurate, as well as to fix the applicators in place so they will not fall out during the planning and treatment. This entire procedure of applicator insertion usually lasts about 1 hour.
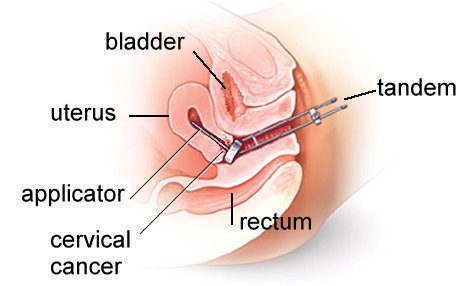
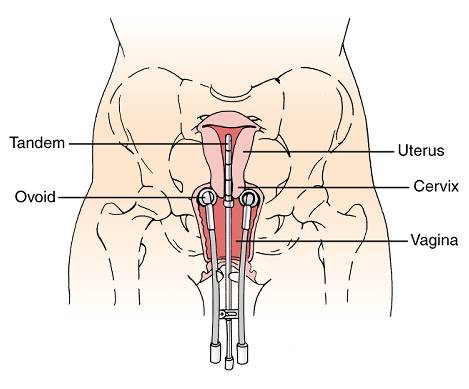
Figure 2 – Diagram showing the positions of the tandem and ovoids in the uterus and vagina from the front (top) and side view (bottom).
Once the applicators are in place, a CT scan is performed to confirm the positions of the applicators, as well as for the radiation oncologist to delineate the tumor and surrounding normal organs ie rectum, sigmoid, bladder, small intestines on every slice of the scan. After this has been done, a radiotherapy plan will be generated to target the tumor with the desired dose, while taking care to minimize damage to the normal organs (Figure 2). The process of CT scanning and planning takes around 2 hours.
Once the radiation oncologist has approved the plan, brachytherapy treatment will commence. During the treatment, a radiation source will be inserted through the hollow tube in the applicators for pre-set amounts of time according to the brachytherapy plan (Figure 3). The patient will not feel anything during the treatment, which is usually completed within 15-30 minutes. Once the treatment is completed, the brachytherapy applicators will be removed.
As there are no radiation sources left in the body after treatment, the patient will not be radioactive and do not need to distance themselves from their family members, children, or pregnant women once the treatment is over. In total, approximately 3 to 5 brachytherapy treatments/insertions will be required to achieve the required curative doses for cervical or uterine cancer.
Single-Channel or “Simple” Brachytherapy
Single-Channel brachytherapy for gynaecological cancers is usually performed after surgery involving removal of the uterus, cervix and part of the upper vagina. What remains of the vaginal canal is sutured closed by the gynaecologist to form the vaginal vault. As the area at highest risk of recurrence is the vaginal vault (being the part that was closest to the original tumor), in many cases, a post-operative course of simple brachytherapy will be performed to reduce the risk of local recurrence. This is usually timed to occur approximately 6 to 8 weeks after surgery, or in cases where combination treatment is indicated, after the respective courses of post-operative EBRT and/or chemotherapy.
Single-channel brachytherapy refers to the requirement for only a single applicator for treatment. As only the vaginal vault remains after surgery, only a single vaginal cylinder is usually required to deliver the brachytherapy (see Figure 4). The insertion of the cylinder is a simpler process than in multi-channel brachytherapy and is relatively painless. After checking that the vaginal vault has healed well following surgery, the radiation oncologist will first measure the length and diameter of the vaginal canal and select the appropriate size of vaginal cylinder. After the cylinder has been assembled, it will be inserted gently into the vagina and up against the vaginal vault. Packing is usually not required as the cylinder is expected to sit comfortably tight in the vaginal canal to minimize air spaces and ensure accurate radiation delivery.
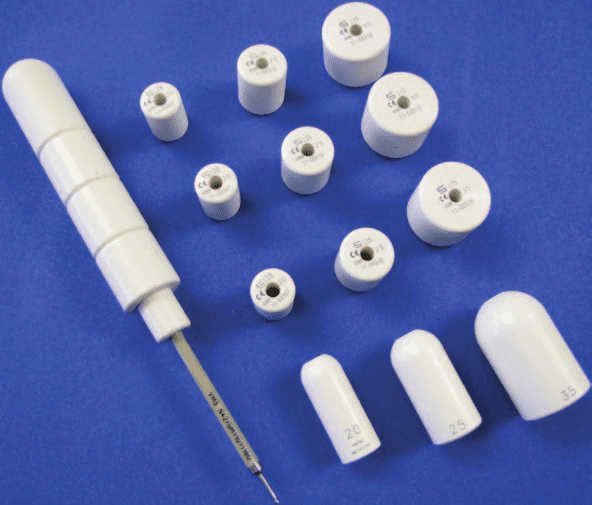
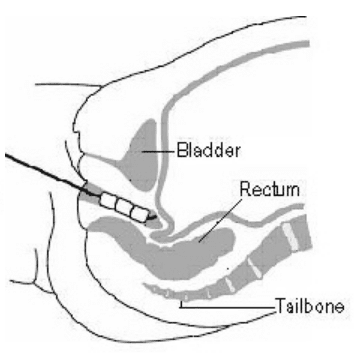
Figure 4 – Picture of vaginal cylinder and the various sizes that can be assembled depending on the measured length and diameter of the vaginal cavity (left) and diagram of the cylinder inserted into the vagina (right).
The patient will proceed for a CT scan after insertion of the vaginal cylinder. Radiotherapy planning and treatment delivery will then follow in a similar process as described for multichannel brachytherapy above.
Meet Our Specialist

Dr. David Tan Boon Harn
Stereotactic Radiosurgery (SRS/SBRT), Gynaecological, Gastrointestinal & Lung Cancers
