Gordon had been living a healthy, active life when he received news that would change his life as he knew it forever. Faced with a prostate cancer diagnosis, he was determined to nip the problem in the bud immediately. As an engineer by profession, his problem solving skills determined that the most efficient path to complete remission would be surgery. However, when he was presented with an alternative treatment – Spaceoar and Radiation therapy at AARO – his perspective changed completely.
The Beginning
The beginning of Gordon’s journey started in 2009. At 62, a routine health check showed his Prostate Specific Antigen (PSA) Levels to be something of concern, measuring 4.0 ng/ml at the time. The PSA is a protein made by the prostate gland1 found in the blood. Higher than normal PSA levels in men can be attributed to a number of reasons, including prostate cancer, benign prostatic hyperplasia (BPH), or infection or inflammation of the prostate gland.
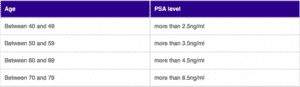
While it is typical for most men to have a PSA level of less than 3ng/ml2, it is normal for the reading to vary from man to man, which typically rises as men grow older. According to the guidelines from Cancer Research UK, a doctor may refer a patient to a specialist if his PSA level is
As an engineer, Gordon liked to chart things to get a clearer picture of how they worked. Based on that initial check up in 2009, he began to track his PSA levels via a graph. He continued to monitor his PSA level until 2013, when his PSA had risen to about 4.6. At that point, his GP advised him to see a urologist.
An uneventful period of regular checkups followed, until 2019, just before the COVID-19 pandemic, when Gordon’s PSA level rose to 7.5. His urologist noted that it was slightly higher than what was considered normal, but after conducting several tests, including a rectal examination, he concluded that the cause of his elevated PSA levels was BPH.
When the COVID-19 pandemic was in full swing, it became much more difficult to schedule regular doctor appointments, so he did miss a few checkups. In one of the subsequent check ups, his PSA level was 9.6. Although he felt completely normal, his urologist was concerned and decided to conduct a more in depth check up. They decided to proceed with an MRI to investigate further. The urologist explained that Gordon
would receive a PIRADS score of 1-5 after the MRI, and that he would probably get a score of 1 or 2.
The Diagnosis
When the MRI results came out, he received a score of PIRADS 5, which raised some alarm bells as it meant he had a high chance of having a significant prostate cancer. A biopsy confirmed that Gordon had prostate cancer with aa Gleason score of 3+4 which amounts to 7. While Gordon initially had no inkling of the implications of this score, after he did a bit more research on Google, he realised that this score indicated that the cancer was significant but with a relatively good prognosis. he was likely to have cancer. At this point, his urologist referred him to an oncologist.
When the results showed that he had stage 2 prostate cancer, Gordon was stunned. All his life, he had been an active person. Ironically, his father and two uncles died at a young age of heart attacks, and so he had always thought that that would be his biggest enemy in life, and that he would have to take special care to avoid contracting a heart attack as he grew older. So, he always looked after his health meticulously. He was fit and active, and closely monitored his blood pressure and cholesterol levels as well.
To receive news like this was like being hit with a sudden bullet. He couldn’t help but wonder how it could have happened. He was overwhelmed by the grim thought that it would not be a heart attack that would kill him, but cancer.
Gordon was most worried that the cancer might spread to other areas, so he sought to receive treatment for his cancer as soon as possible. As soon as the next appointment was available, he and his wife were at the oncologist’s office to seek an opinion.
Looking back, Gordon believes that the oncologist was probably highly influenced by Gordon. When he arrived, instead of listening to all the available treatment options, Gordon already had in mind how he wanted to be treated.
With his own background in engineering, he was taught that any structural component that is faulty or old or cracked has to be cut out and removed, so his approach to his cancer treatment mirrored such strategies. To him, there was only one way to go about obtaining cancer treatment, and that was surgery. He had not really understood the full extent of the complications from surgery, but when the oncologist had explained that while there would be dark clouds on the horizon, but a cure was definitely available, he and his wife were filled with mutual relief. Gordon recalls that they both shared the thought, “Oh, that’s good news!” When the oncologist asked him what he thought about the treatment options, Gordon firmly insisted that a surgical procedure with a robot would be his only option, and the oncologist agreed to proceed with that course of treatment.
At that point, the oncologist referred Gordon back to his urologist because his urologist was a surgeon too, and the oncologist believed that his urologist could conduct the surgery or recommend someone else to conduct the surgery.
However, the urologist was unexpectedly opposed to this turn of events. When Gordon expressed his desire to undergo the surgery, the urologist strongly discouraged him from doing so. The doctor urged him, “Please don’t do that, I’m a surgeon and I’m advising you not to do surgery because the risks are just too high.” The urologist even called the oncologist from the examination room, and explicitly told the latter that he
disagreed with this course of treatment. Instead, he requested for the oncologist to recommend a radiation specialist instead to see what else could be done.
Through this process, Gordon was recommended to Dr Jonathan.
Embarking on Radiation Therapy
Gordon’s first impression of Dr Jonathan was formed even before the latter introduced himself. When he and his wife were in the waiting room, they saw a youthful man walk past them in the waiting area and enter a consultation room. Gordon felt that he seemed pleasant and upright, and turned to his wife and said, “I hope this is the guy we’re going to talk to!” And as it turned out, that upright, pleasant man did turn out to be Dr Jonathan.
When they entered the consultation, Gordon and his wife were still quite keen on the surgery, but had proceeded with the consultation to appease his urologist. However, that one consultation completely changed Gordon’s perspective.
During the consultation, Dr Jonathan drew what Gordon now refers to affectionately as “potato diagrams” with arrows that clearly showed how the various radiation treatment options would work and their pros and cons. It was as though Gordon had a lightning bolt of clarity, as he was able to understand exactly how the proposed treatment would work. Before this consultation, he had not even heard about Stereotactic body radiotherapy (SBRT) because he had been so bent on surgery that he had not taken the time to explore other options.
When it was clearly explained to Gordon, SBRT seemed like a miracle solution to him. Despite the side effects, they could be mitigated, and the timeline drawn for him was four weeks from start to finish. Gordon shared “ This meant that I could carry on with my life and do anything I like before and afterwards. After the consultation, my wife and I went home and did more research, which confirmed that it was a really good option with a short treatment time and little side effects”. The next day, they contacted AARO and confirmed that they were keen to proceed.
While he had heard of other options for radiation, such as brachytherapy, he decided against it because he did not like the idea of having permanent implants within his prostate. As an active golfer and sportsperson, Gordon was keen to return to his regular schedule of activities,
and did not want to endure a longer course of treatment with a conventional schedule of daily radiation sessions for up to 8 weeks. Furthermore, through his discussion with Dr Jonathan, he realised that there was no significant difference between opting for a lower dose for longer periods of time and a higher dose for a shorter period of time in his particular treatment plan, so the SBRT treatment seemed to be optimal. “And this made the decision to go with SBRT a no-brainer for me”, he said with a smile.
Hydrogel Spacer in Prostate Cancer Treatment
Perhaps the only facet of the treatment plan that Gordon could not quite comprehend was the fact that the space oar or hydrogel would be inserted into his backside, between the prostate and the retinal wall. Gordon was concerned that the presence of a gelliquid within a space that would otherwise be empty would be quite uncomfortable. However, after discussions about this with Dr Jonathan, Gordon was reassured that it would not be as bad as it seemed.
Hydrogel spacer insertion for rectal protection prior to radiation had been introduced relatively recently in Singapore. The concept is simple but elegant – injection of a biodegradable material that creates space between the prostate and rectum to spare the rectum from high dose radiation, which then dissolves away after it is not needed. Medical studies show that long term rectal bleeding risks from radiotherapy are significantly reduced by the procedure. Dr Jonathan offers this routinely to all suitable patients, and because just one needle insertion is required, it can be done under local anesthesia.
For Gordon, he found that the most miraculous aspect of the hydrogel was that it would dissolve on its own, and did not have to be removed via a surgical procedure. With the foreknowledge that the prostate was quite near the rectal wall, which thus caused it to be easily damaged during the course of traditional treatments such as surgery, the fact that the hydrogel spacer treatment could mitigate the risk of damage made it seem amazing.
The hydrogel spacer procedure went smoothly although he did experience some discomfort in his back from the rectal ultrasound probe required to guide the needle into place. But it was nothing he could not bear and the needle insertion itself was painless with the local anesthesia. The planning scans a week later delighted Dr Jonathan – up to 1 cm of space was created between prostate and rectum and planning was going to be a breeze. An extremely ‘rectum-friendly’ plan was created, making the short procedure all worthwhile for Gordon.
Reflecting on the treatment process, Gordon recalls that the most uncomfortable aspect was the ultrasound of the back passage. But considering the results of the procedure, Gordon affirmed that the discomfort was worth it.
In his recollection of side effects of his treatment, there were a few short term side effects of treatment, but they were resolved quite quickly. He experienced a little bit of bleeding from the anus, but he was reassured by Dr Jonathan and the staff that this was a short term side effect. After it was resolved in a few days, Gordon did not experience any other major symptoms. During the treatment, his bowel movements were also more
frequent, but about a month after treatment, he managed to establish a routine for his bowel movements, and they have become much more regular.
Perhaps the most significant long term side effect of treatment is that Gordon now experiences slight discomfort with urination because it takes about 3-4 seconds for urine to come through, whereas it used to be instantaneous. He also has some difficulty emptying his bladder all at once, but he has developed coping strategies to deal with these inconveniences. For instance, he has learnt that holding on to his urge to urinate can make the actual process of urination much easier.
Immediately after treatment, Gordon took Flowmax and another medication that reduced the number of times Gordon had the urge to urinate but since then, Gordon has managed to wean himself off both of them. Dr Jonathan pointed out that some of these side effects may only be resolved after about 12 months, and Gordon readily accepts this, as these are only minor adjustments to my daily life that he has to make to cope with these things.
These days, Gordon is able to enjoy his life to the fullest. Prior to the interview, he had just returned from a ski trip. As early as three weeks after the radiation treatment, he was able to be back tinkering with his boat, playing golf and pickle ball and all the other outdoor activities. His urinary flows and other activities remain generally unaffected, and he regards this to be a sign that everything has generally returned to its normal functions. Besides some minor adjustments, such as paying attention to his urges to use the toilet and ensuring that there is a toilet within reach at all times, he does not experience any other inconveniences to his daily life.
Closing Thoughts
The most important takeaway from this experience, for Gordon, is the importance of annual checkups. He notes that 1 in 8 people might be faced with a diagnosis like his and early prostate cancer is virtually undetectable unless there are regular checkups conducted. “When I spend time with my friends, I often remind them to go get their health checked regularly”, he says with a chuckle, and adds that he is determined to raise awareness of prostate cancer.
A second, and equally important takeaway for him was that the support of friends and family around him was vital to his recovery. Through the process of recovery, his wife was a constant pillar of support, and he actually grew closer to friends who encouraged him along his journey.
Lastly, he was reminded that everyone is human and therefore fallible. No matter how healthy you might perceive yourself to be, there is always the possibility of encountering a disease like this. He wakes up each day, and is thankful that he is able to go about his activities as per normal.
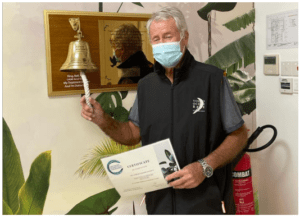
Gordon extends his gratitude to the staff at AARO and Dr Jonathan. Initially, his wife had decided to accompany him for every trip to the Centre for Stereotactic Radiosurgery (CSR) for radiation treatment, but after the first few sessions, he felt completely comfortable in the environment and told her that it was not necessary. The staff were warm and always meticulously attended to the needs of all the patients. Every step of the process became a part of a familiar routine that offered reassurance in its regularity. “I think the environment here is so unique because it isn’t too crowded, and it’s easy to find parking, for instance, and after a while it becomes like a second home of sorts”.
The Prostate SBRT itself was routine and straightforward as Dr Jonathan had done countless targeting sessions before, having been the Principal Investigator of Southeast Asia’s first clinical trial for Prostate SBRT in 2015. One thing Dr Jonathan found since using the rectal spacers was that it also helped stabilize the prostate position, making the targeting procedure even easier. The week and a half of treatment proceeded smoothly for both doctor and patient.
Dr Jonathan commented, “Gordon approached his cancer diagnosis with calmness and determination. Once presented with all his treatment options he took the effort to understand them, and once he made his decision based on the rationale of non-invasiveness and safety, he went ahead with full confidence. His wife was a constant pillar of support that he could count on. It was gratifying to hear that he returned to all his usual sporting activities shortly after and was whizzing down ski slopes like before. Gordon leveraged the latest minimally invasive technologies to achieve his desired outcome of living life to the full despite the dreaded big ‘C’ diagnosis.”
This season, we are privileged to celebrate our Ambassador of Hope: Gordon.
1 Definition from the National Cancer Institute
https://www.cancer.gov/publications/dictionaries/cancer-terms/def/psa
2 Figures from Cancer Research UK
https://www.cancerresearchuk.org/about-cancer/tests-and-scans/prostate-specific-antigenpsatest#:~:text=Typically%2C%20most%20men%20have%20a,be%20normal%20in%20older%20men.